Abstract
Fanconi anemia (FA) is an inherited disorder associated with loss of function mutations in gene members of the FA-BRCA pathway involved in interstrand cross-link DNA damage repair during cell division. Progressive bone marrow failure (BMF) is a primary cause of morbidity and mortality in patients with FA. Allogeneic hematopoietic stem and progenitor cell (HSPC) transplantation is the only curative treatment for FA-associated BMF. However, donor availability, graft failure, and FA-specific transplant toxicities remain significant hurdles. Attempts at genetic correction of FA are underway but collection of sufficient numbers of autologous HSPCs is challenging in subjects with advanced BMF. Androgens have been successfully used but side effects often prevent prolonged therapy. The orally bioavailable small molecule mimetic of thrombopoietin, eltrombopag (EPAG), was recently shown to stimulate multipotent long-term repopulating HSPCs in patients with acquired BMF, resulting in persistent trilineage hematopoiesis. EPAG promotes DNA repair (Guenther, Exp Hematol 2019) and maintains HSPCs under inflammatory conditions (Alvarado, Blood 2019), indicating potential relevance in FA. In this study, we investigated whether EPAG may offer a novel therapeutic modality for FA-associated BMF.
We have enrolled 10 patients (FANCA, n=9 and FANCC, n=1) to date in a prospective phase I/II study of EPAG in Fanconi anemia (NCT03204188). All subjects received EPAG at an oral daily dose adjusted for age and ethnicity. The primary efficacy endpoint was the proportion of subjects with at least 2-fold increase in marrow cellularity or CD34+ HSPC frequency (marrow response), or clinically significant improvement in peripheral blood (PB) counts at 6 months (blood response). The primary safety endpoint was the global toxicity profile assessed at 6 months using CTCAE criteria. Responders were invited to continue on the extension phase of the study for an additional 3 years.
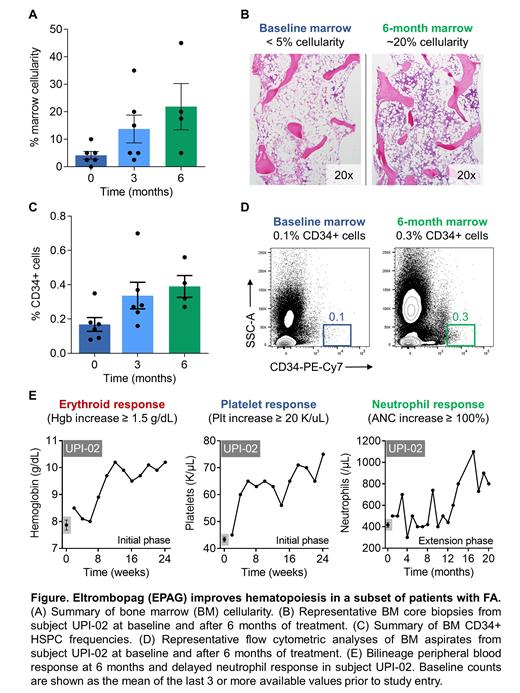
Four of 10 patients have reached the 6-month assessment endpoint, and a pre-specified 3-month interim analysis is available on two additional subjects. A marrow response was observed in all 4 subjects at 6 months. Mean marrow cellularity increased by a factor of 4 (Fig. A/B), and CD34+ HSPC frequency improved 2.5-fold at 6 months relative to pre-treatment values (Fig. C/D). Marrow response criteria were also met in the other two subjects at the 3-month interim assessment. Primary PB response was observed in 2 of 4 patients in one (hemoglobin) or two lineages (hemoglobin and platelets) at 6 months of treatment. Responders continue to receive EPAG at 10 or 25 months with sustained improvements in blood counts and transfusion independence. The subject treated for 25 months recently met response criteria in a third lineage (neutrophils) (Fig. E). Both patients who had a marrow but no PB response are clinically well; one subject (FANCA) underwent an unrelated allogeneic HSPC transplantation one year ago, and the other subject (FANCC) recently entered the extension phase of this study. Unilineage PB response criteria were also met in one of two subjects at the 3-month interim assessment.
No drug-related serious adverse events have occurred during EPAG treatment. All patients tolerated the maximum dose of EPAG and no interruption or dose reduction was required for adverse events attributable to EPAG. Patients without transfusional iron overload at study entry developed progressive depletion of iron stores attributable to the known potent iron chelating and mobilizing properties of EPAG. At a median of 3 months after initiating EPAG (range, 1 to 6 months), affected patients initiated daily oral iron supplementation with gradual amelioration of iron store levels. To date, there has been no occurrence of marrow fibrosis, solid malignancies or clonal evolution, defined as abnormalities on standard metaphase analysis of bone marrow or overt clinical transformation to MDS/AML.
In sum, treatment with EPAG was associated with increased marrow HSPCs in all subjects and PB responses in a subset of patients with Fanconi anemia. The overall safety profile was favorable. Further follow-up and expansion of the ongoing patient cohort will confirm EPAG's potential as a safe and efficient long-term therapeutic modality for FA-associated BMF. Alternatively, EPAG could also be used safely to boost marrow CD34+ cell numbers prior to autologous gene therapy applications.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal